How to Identify Male Cyclists at Risk of RED-S?
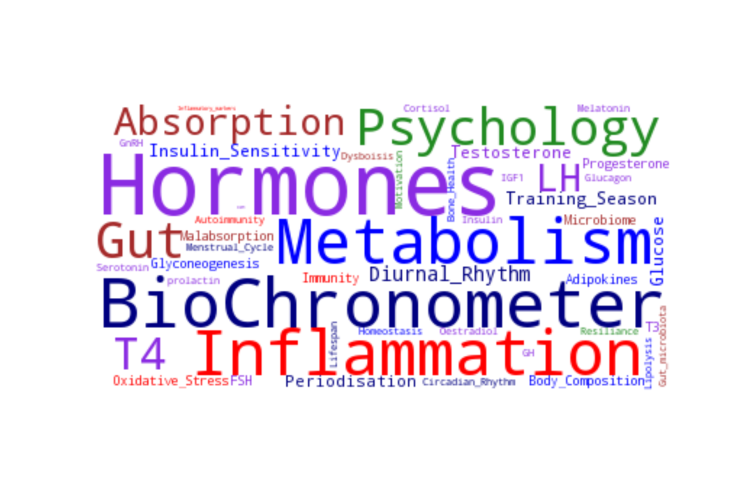
Relative energy deficiency in sport (RED-S) is a clinical model that describes the potential adverse health and performance consequences of low energy availability (LEA) in male and female athletes. Identification of athletes at risk of LEA can potentially prevent these adverse clinical outcomes.
Athletes at risk of RED-S are those involved in sports where low body weight confers a performance or aesthetic advantage. In the case of competitive road cycling, being light weight results in favourable power to weight ratio to overcome gravity when cycling uphill. How can male cyclists at risk of LEA be effectively identified in a practical manner?
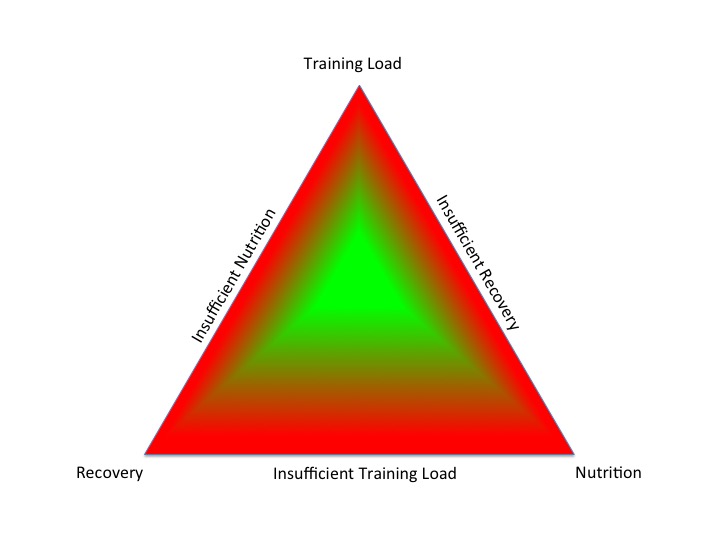
Energy availability (EA) is defined as the residual energy available from dietary intake, once energy expenditure from exercise training has been subtracted. This available energy is expressed as KCal/Kg fat free mass (FFM). A value of 45 KCal/Kg FFM is roughly equivalent to basal metabolic rate, in other words the energy required to sustain health. In order to quantify EA, accurate measurements of energy intake and expenditure, and FFM assessed from dual X ray absorptiometry (DXA), need to be undertaken. However this is not practical or feasible to undertake all these measurements outside the research setting. Furthermore, methodology for assessing energy intake and expenditure is laborious and fraught with inaccuracies and subjectivity in the case of diet diaries for “free living athletes“. Even if a value is calculated for EA, this is only valid for the time of measurement and does not give any insights into the temporal aspect of EA. Furthermore, an absolute EA threshold has not been established, below which clinical symptoms or performance effects of RED-S occur.
Self reported questionnaires have been shown to be surrogates of low EA in female athletes. However there are no such sport specific questionnaires, or any questionnaires for male athletes. Endocrine and metabolic markers have been proposed as quantitative surrogate measures of EA and shown to be linked to the RED-S clinical outcome of stress fractures in runners. In female athletes the clinical sign of regular menstruation demonstrates a functioning H-P ovarian axis, not suppressed by LEA. What about male athletes? Although hypothalamic suppression of the reproductive axis due to LEA can result in low testosterone, high training loads, in presence of adequate EA, can lead to the same negative effect on testosterone concentration.
Male cyclists present a further level of complexity in assessing EA status. In contrast to runners, stress fracture will not be an early clinical warning sign of impaired bone health resulting from low EA. Furthermore cyclists are already at risk of poor bone health due to the non weight bearing nature of the sport. Nevertheless, traumatic fracture from bike falls is the main type of injury in cycling, with vertebral fracture requiring the longest time off the bike. Chris Boardman, a serial Olympic medal winner in cycling, retired in his early 30s with osteoporosis. In other words, in road cycling, the combined effect of the lack of osteogenic stimulus and LEA can produce clinically significant adverse effects on bone health.
What practical clinical tools are most effective at identifying competitive male cyclists at risk of the health and performance consequences of LEA outlined in the RED-S model? This was the question our recent study addressed. The lumbar spine is a skeletal site known to be most impacted by nutrition and endocrine factors and DXA is recognised as the “gold standard” of quantifying age matched Z score for bone mineral density (BMD) in the risk stratification of RED-S. What is the clinical measure indicative of this established and clinically significant sign of RED-S on lumbar spine BMD? Would it be testosterone concentration, as suggested in the study of runners? Another blood marker? Cycle training load? Off bike exercise, as suggested in some previous studies? Clinical assessment by interview?
Using a decision tree approach, the factor most indicative of impaired age matched (Z score) lumbar spine BMD was sport specific clinical assessment of EA. This assessment took the form of a newly developed sports specific energy availability questionnaire and interview (SEAQ-I). Reinforcing the concept that the most important skill in clinical medical practice is taking a detailed history. Questionnaire alone can lead to athletes giving “correct” answers on nutrition and training load. Clinical interview gave details on the temporal aspects of EA in the context of cycle training schedule: whether riders where experiencing acute intermittent LEA, as with multiple weekly fasted rides, or chronic sustained LEA with prolonged periods of suppressed body weight. Additionally the SEAQ-I provided insights on attitudes to training and nutrition practices.
Cyclists identified as having LEA from SEAQ-I, had significantly lower lumbar spine BMD than those riders assessed as having adequate EA. Furthermore, the lowest lumbar spine BMD was found amongst LEA cyclists who had not practised any load bearing sport prior to focusing on cycling. This finding is of particular concern, as if cycling from adolescence is not integrated with weight bearing exercise and adequate nutrition when peak bone mass (PBM) is being accumulated, then this risks impaired bone health moving into adulthood.
Further extension of the decision tree analysis demonstrated that in those cyclists with adequate EA assessed from SEAQ-I, vitamin D concentration was the factor indicative of lumbar spine BMD. Vitamin D is emerging as an important consideration for athletes, for bone health, muscle strength and immune function. Furthermore synergistic interactions with other steroid hormones, such as testosterone could be significant.
What about the effects of EA on cycling performance? For athletes, athletic performance is the top priority. In competitive road cycling the “gold standard” performance measure is functional threshold power (FTP) Watts/Kg, produced over 60 minutes. In the current study, 60 minute FTP Watts/Kg had a significant relationship to training load. However cyclists in chronic LEA were under performing, in other words not able to produce the power anticipated for a given training load. These chronic LEA cyclists also had significantly lower testosterone concentration. Periodised carbohydrate intake for low intensity sessions is a strategy for increasing training stimulus. However if this acute intermittent LEA is superimposed on a background of chronic LEA, then this can be counter productive in producing beneficial training adaptations. Increasing training load improves performance, but this training is only effective if fuelling is tailored accordingly.
Male athletes can be at risk of developing the health and performance consequences of LEA as described in the RED-S clinical model. The recent study of competitive male road cyclists shows that a sport specific questionnaire, combined with clinical interview (SEAQ-I) is an effective and practical method of identifying athletes at risk of LEA. The temporal dimension of LEA was correlated to quantifiable health and performance consequences of RED-S.
References
Low energy availability assessed by a sport-specific questionnaire and clinical interview indicative of bone health, endocrine profile and cycling performance in competitive male cyclists Keay, Francis, Hind, BMJ Open in Sport and Exercise Medicine 2018
2018 UPDATE: Relative Energy Deficiency in Sport (RED-S) Keay, BJSM 2018
Fuelling for Cycling Performance Science4Performance
Pitfalls of Conducting and Interpreting Estimates of Energy Availability in Free-Living Athletes International Journal of Sport Nutrition and Exercise Metabolism 2018
IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update BJSM 2018
Low Energy Availability Is Difficult to Assess but Outcomes Have Large Impact on Bone Injury Rates in Elite Distance Athletes International Journal of Sport Nutrition and Exercise Metabolism 2018
Treating exercise-associated low testosterone and its related symptoms The Physician and Sports Medicine 2018
Male Cyclists: bones, body composition, nutrition, performance Keay, BJSM 2018
Cyclists: Make No Bones About It Keay, BJSM 2018
Male Athletes: the Bare Bones of Cyclists
Cyclists: How to Support Bone Health?
Synergistic interactions of steroid hormones Keay BJSM 2018
Fuel for the Work Required: A Theoretical Framework for Carbohydrate Periodization and the Glycogen Threshold Hypothesis Sports Medicine 2018